2025 AADA Legislative Conference: Medicare payment background

Medicare Physician Payment Reform: Ensure Medicare stability for patients and physicians
Medicare physician payment has failed to keep up with inflation, threatening the viability of medical practices. The current payment structure has contributed to consolidation and increased hospital ownership of physician practices, which are more costly, reduce competition, and are less patient-centered. Annual cuts to Medicare payment jeopardize physicians’ ability to keep the doors open and care for patients in our communities.
Legislative ask
Take action to address the systemic issues within the Medicare physician payment system and safeguard physicians’ ability to provide patient access to care. We urge Congress to:
House:
Senate:
Cosponsor S. 1640, the Medicare Patient Access and Practice Stabilization Act of 2025, which reverses the 2025 2.83% cut and provides a positive inflationary adjustment for physician practices for 2025.
Continue to work towards long-term Medicare Physician Payment reform.
Messaging for Congressional visits
Message to Capitol Hill
As a dermatologist, I am deeply concerned that the Medicare Physician Fee Schedule fails to reimburse physician practices adequately and threatens access to care for patients in our community. Medicare payment for physicians is not linked to inflation, yet facilities like hospitals and skilled nursing facilities receive annual inflationary updates.
In 2025, the Centers for Medicare & Medicaid Services (CMS) cut physician reimbursement by 2.83%. Congress failed to reverse this cut at the end of 2024. This is in addition to cuts to Medicare physician payments over the past five years that total over 10%. While Congress thankfully provided a payment update for 2026, there has not been a resolution to the 2025 cuts, so Congress should act to address the 2025 cuts while continuing to work on long-term Medicare Physician Payment reform that takes into account the realities facing physicians with record inflation, skyrocketing practice expenses, and workforce shortages.
Messaging tips
Use this opportunity to personally demonstrate the value of care in the dermatologist’s office setting.
Example: Compare the cost of treating your patient with melanoma or another complex skin disease in your office as opposed to an outpatient hospital setting and explain how treating your patient in your office is also better for patient outcomes.
Personalize how lack of adequate payment impacts your ability to maintain high-quality staff and, specifically, jobs in your community.
Example: Remind them your practice contributes to the economy in their community and their constituents. Explain that other industries have the flexibility to change the pricing of their products to reflect rising costs and increase staff salaries, while physicians do not have that ability because the Medicare Physician Fee Schedule sets the rate of reimbursement. What other profession or business would be able to sustain operating under such a structure?
Issue background
H.R.879 and S.1640 would eliminate the 2.83% cut to Medicare physician payment that physicians received on January 1, 2025. The legislation also includes an inflationary increase of 2% which is roughly half of the Medicare Economic Index (MEI) for 2025.
H.R.879 and S.1640 are expected to cost approximately $3.8 billion.
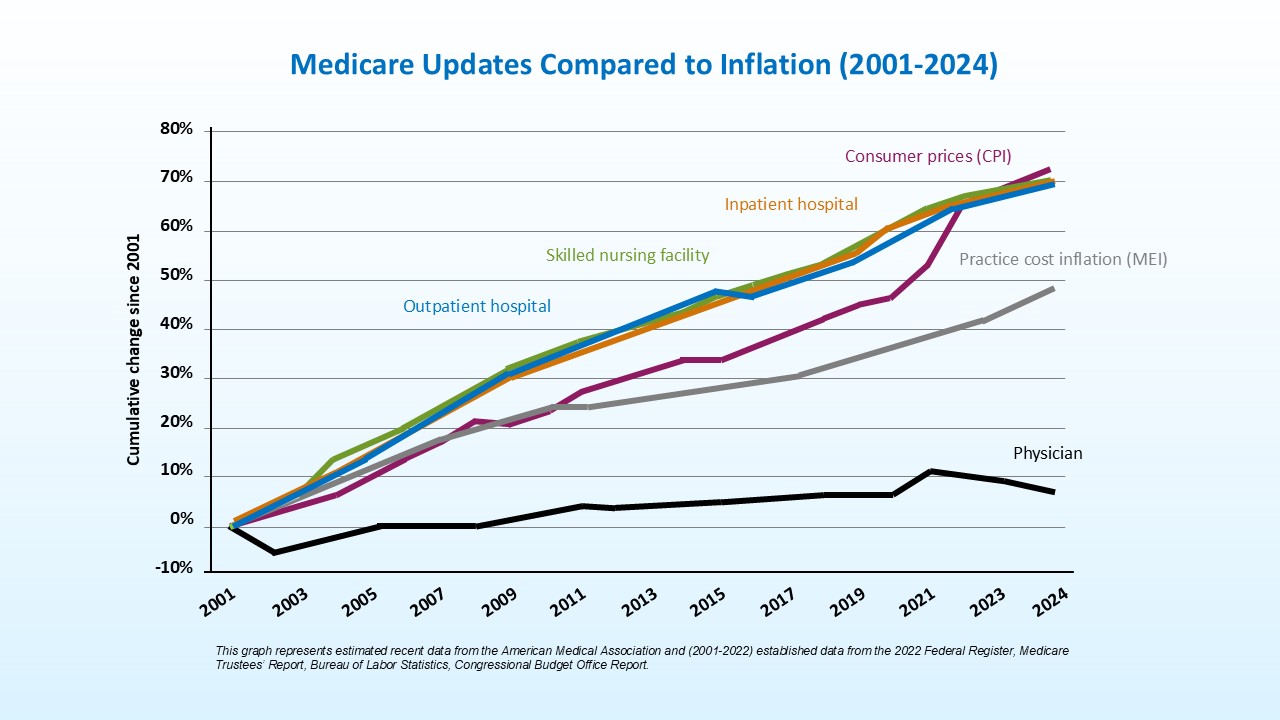
Since 2001, the cost of operating a medical practice has increased by 59%, while Medicare physician payment has decreased by 33% when adjusted for inflation.
This out-of-balance payment structure disproportionately threatens the viability of medical practices, especially smaller, independent, physician-owned practices, as well as those serving low-income or historically marginalized patients.
The current Medicare physician payment system has led to increased consolidation and hospital ownership of physician practices resulting in higher expenses and reduced competition to the health care system.
Physician practices rely on reimbursement to cover a multitude of practice expenses including:
Staff salaries and benefits
The cost of federal and state regulatory compliance
The costs associated with insurance mandates such as step therapy and prior authorization.
Annual cuts to Medicare physician reimbursement jeopardize our ability to keep our doors open and care for patients in our communities. Many physicians have already had to close their doors, leave their communities, retire early, or leave the practice of medicine. The inability to provide inflationary pay raises to practice employees is contributing to the current health care workforce crisis in which we are seeing increasing burnout rates and a mass exodus of our clinical, administrative, and clerical staff into other industries.
With reduced staff comes diminished capacity to provide quality health care and maintain patient access. Reduced staffing leads to barriers in communicating and coordinating care, such as scheduling appointments and discussing laboratory reports, which can impact patient satisfaction and outcomes.
Fewer physicians in our communities means longer waiting times for patients to receive care. When those patients do receive care, their only option may be clinical staff with less training, or more expensive care in suboptimal settings including emergency departments and hospital-based practices.
Medicare patients will suffer in the end with delayed and second-rate care at a higher cost.
Recent updates
In July 2025, Congress passed H.R.1, the One Big Beautiful Bill Act. The legislation provides for a one-year 2.5% increase to Medicare physician payment in 2026 to account for sustained cuts as Congress continues to work toward long-term payment reform. This short-term remedy is only applicable to 2026 – a fix for 2025 in addition to long-term reform is still needed.
Physician groups are not alone in calling for increases to Medicare physician payment. The Medicare Payment Advisory Commission (MedPAC), a nonpartisan independent legislative branch agency that provides the US Congress with analysis and policy advice on the Medicare program, has also called for physician payment to be tied to inflation.
In 2025, MedPAC recommended that Congress replace the current-law updates to the Medicare Physician Fee Schedule with annual updates tied to a portion of MEI such as MEI minus 1 percent.
The goal of the recommendation is to maintain physician participation in Medicare. MedPAC projects this change would increase federal spending by $15 to 30 billion dollars over five years and raise beneficiary premiums and cost-sharing.
MedPAC also stated that they are concerned about whether beneficiaries will continue to have adequate access to care in the coming years as growth in physician practice operating costs is expected to exceed growth in Medicare payment rates by a greater amount than it did in the prior two decades. This larger gap could create incentives for physicians to reduce the number of Medicare beneficiaries they treat, stop participating in Medicare entirely, or vertically consolidate with hospitals, which could increase spending for beneficiaries and the Medicare program.
The momentum for Medicare physician payment reform is growing. Help by sharing your own experience when you’re on Capitol Hill.
Pre-conference reading
Check out additional resources and reading material:
American Medical Association: Five years of decline in Medicare conversion factor
This chart shows how the Medicare conversion factor has declined by more than 10% over the last five years.American Medical Association: Payment updates chart
This chart shows Medicare payment updates across various providers including hospitals, skilled nursing facilities, and physicians.Kaiser Family Foundation: Timeline: History of health reform in the U.S.
Kaiser Family Foundation: What to know about how Medicare pays physicians
American Medical Association: Merit-based incentive payment system (MIPs) primer
 Find a Dermatologist
Find a Dermatologist
 Member directory
Member directory
 AAD Learning Center
AAD Learning Center
 2026 AAD Annual Meeting
2026 AAD Annual Meeting
 Need coding help?
Need coding help?
 Reduce burdens
Reduce burdens
 Clinical guidelines
Clinical guidelines
 Why use AAD measures?
Why use AAD measures?
 Latest news
Latest news
 New insights
New insights
 Physician wellness
Physician wellness
 Joining or selling a practice?
Joining or selling a practice?
 Promote the specialty
Promote the specialty
 Advocacy priorities
Advocacy priorities
