What is Mohs surgery?
Also called Mohs micrographic surgery
Used to treat skin cancer, this surgery has a unique benefit. During surgery, the surgeon can see where the cancer stops. This isn’t possible with other types of treatment for skin cancer.
The ability to see where the cancer stops gives Mohs (pronounced Moes) two important advantages:
Mohs has a high cure rate.
Mohs allows you to keep as much healthy skin as possible because the surgeon only removes the skin with cancer cells. This is especially important when skin cancer develops in an area with little tissue beneath (e.g., eyelid, ear, or hand).
What is it like to have Mohs surgery?
If you have Mohs surgery, you’ll see a doctor who is a trained Mohs surgeon. Most Mohs surgeons are dermatologists who have completed extensive training in Mohs surgery.
During Mohs surgery, most patients remain awake and alert. This means Mohs can safely be performed in a medical office or surgical suite. Only if extensive surgery is necessary would you be admitted to a hospital.
On the day of the surgery, your surgeon will first examine the area to be treated. You’ll then be prepped for surgery. This includes giving you an injection of anesthetic. This injection only numbs the area that will be operated on, so you’ll be awake during the surgery.
Once the anesthetic takes effect, the surgery can begin. The surgeon starts by first cutting out the visible skin cancer. Next, the surgeon removes a thin layer of surrounding skin. You’re then bandaged so that you can wait comfortably.
While you wait, the Mohs surgeon looks at the removed skin under a microscope. The surgeon is looking for cancer cells. If cancer cells are found, you’ll need another layer of skin removed.
This process of removing a thin layer of skin and looking at it under a microscope continues until the surgeon no longer sees cancer cells.
Once cancer cells are no longer seen, your surgeon will decide whether to treat your wound. Some wounds heal nicely without stitches. Others need stitches. To minimize the scar and help the area heal, some patients require a skin graft or other type of surgery.
If you need wound treatment, your Mohs surgeon may treat the wound that same day. Some patients with a large wound are referred to another surgeon for wound treatment.
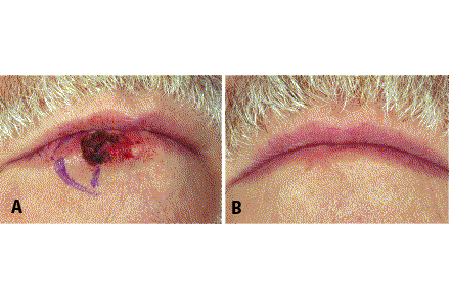
Some wounds heal without stitches
A: The Mohs surgeon didn’t stitch the wound on this man’s lip.
B: 6 weeks later, the wound has healed on its own.
When is Mohs surgery recommended?
Most Mohs patients have a common type of skin cancer like basal cell carcinoma (BCC) or squamous cell carcinoma (SCC). Mohs is usually recommended when a BCC or SCC:
Is aggressive or large
Appears in an area with little tissue beneath it (e.g., eyelid, nose, ear, scalp, genitals, hand, or foot)
Was treated and has returned
Mohs is also used to treat some rare skin cancers like DFSP, extramammary Paget’s disease, and Merkel cell carcinoma.
Can Mohs treat melanoma?
Yes, dermatologists occasionally recommend Mohs for treating melanoma, the most serious type of skin cancer. Mohs is only used to treat an early melanoma, and it must be a type of melanoma called lentigo malignant melanoma. This type of melanoma stays close to the surface of the skin for a while.
When treating melanoma, the surgeon uses a modified type of Mohs surgery called slow Mohs. It’s called slow because the patient must wait longer for the results. It’s not possible for the surgeon to look at the removed skin and know right away whether it contains cancer cells. More time is needed.
If you have slow Mohs, the surgeon will remove the visible skin cancer and a bit of normal-looking skin around it. You’ll then be bandaged and sent home.
Most patients return the next day. It’s then that the patient learns whether more skin must be removed or the wound can be closed. Again, some wounds are left to heal on their own.
Who is Mohs recommend for?
No matter what type of skin cancer you have, Mohs is only recommended for certain patients. You must have one skin cancer or a few skin cancers that are very close together.
Mohs patients have good results
Having any type of surgery can be scary. If your dermatologist recommends Mohs, you can take comfort in knowing a few facts. Mohs has a high cure rate. Your surgeon will remove the least amount of skin needed to treat the cancer.
What to expect during Mohs surgery?
Use this infographic to learn what to expect during mohs surgery.
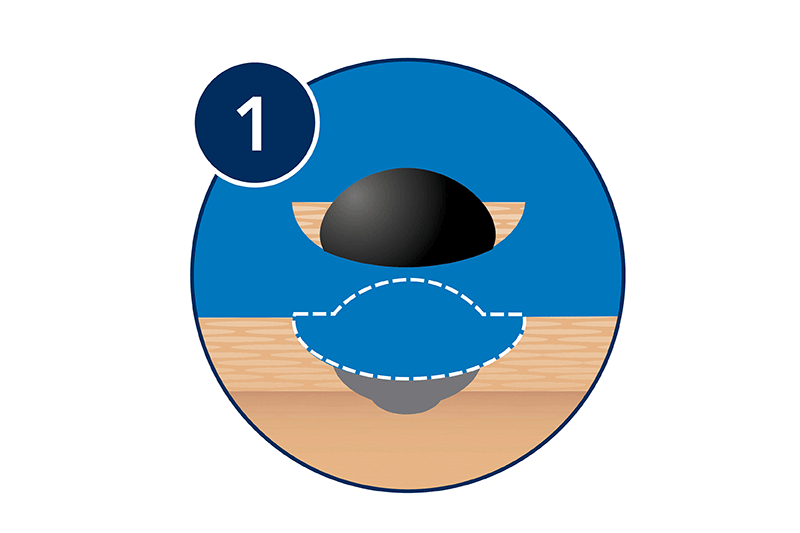
The visible tumor and a thin layer of surrounding skin are removed.
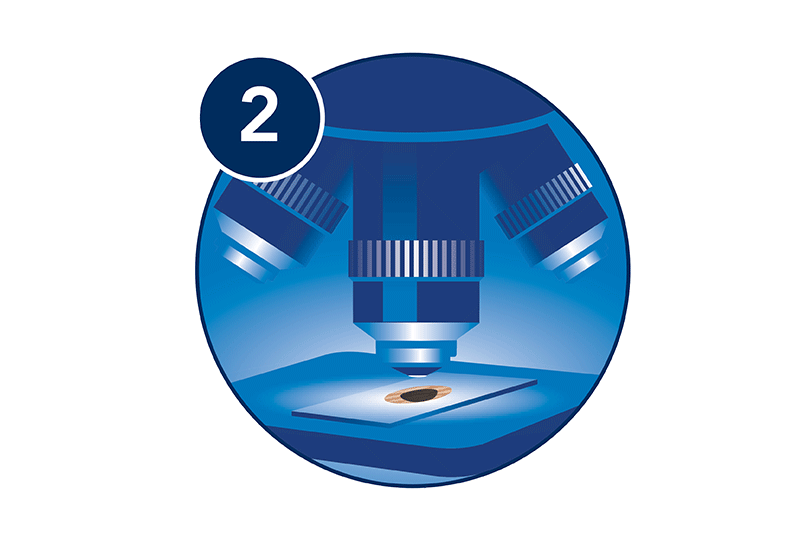
The tissue is examined under a microscope to see if any cancer cells remain at any of the edges.
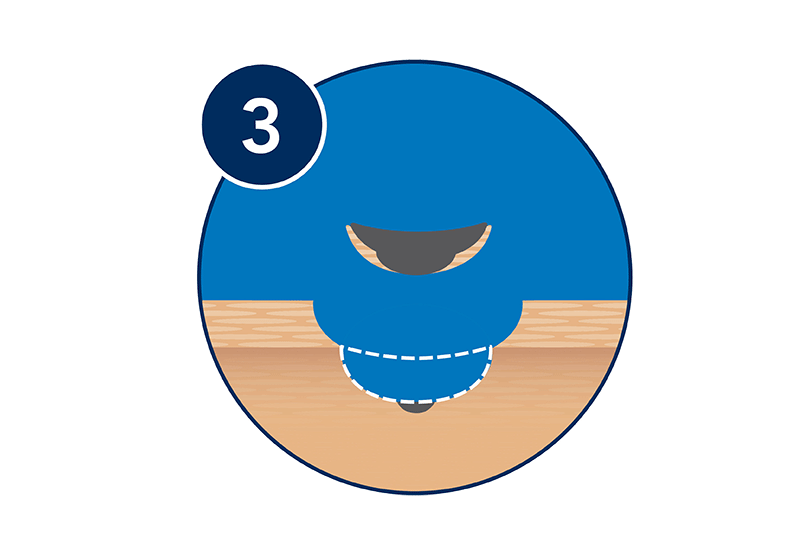
If any cancer cells remain, additional skin is removed and examined under the microscope.
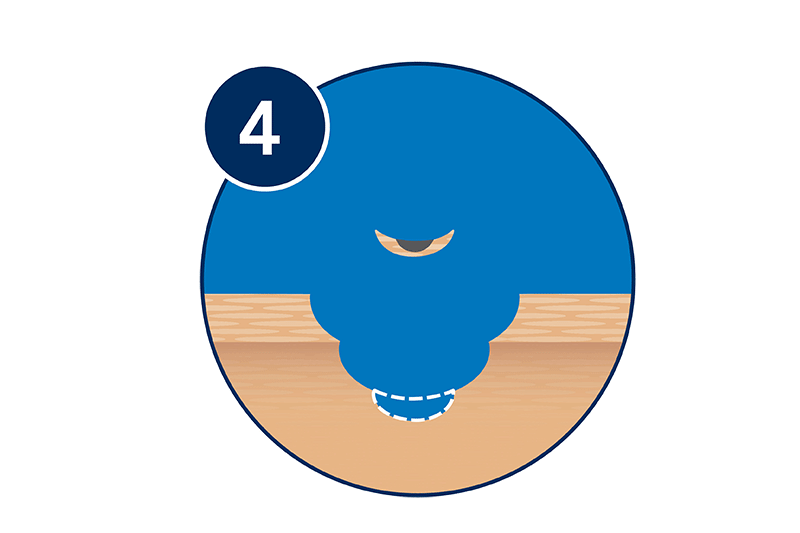
This process continues until no more cancer cells are found at the edges.
Download the "What to expect during Mohs surgery" infographic (PDF).
Images
References
Schaeffer M, Geisler A, et al. “Patient-reported preferences associated with Mohs micrographic surgery of nonmelanoma skin cancer: Relative importance of factors pertaining to surgeons and staff during the perioperative course.” Poster presented at: 74th Annual Meeting of the American Academy of Dermatology; 2016 Mar 4-8; Washington, DC. Commercial support: None identified.
Stigall LE, Brodland DG, et al. “The use of Mohs micrographic surgery (MMS) for melanoma in situ (MIS) of the trunk and proximal extremities.” J Am Acad Dermatol. 2016 Nov;75(5):1015-121.
Walker E, Mann M, et al. “Rapid visualization of nonmelanoma skin cancer.” J Am Acad Dermatol. 2017 Feb;76(2):209-16.
Last updated: 5/17/21
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?