Pictures of basal cell carcinoma
Last updated: October 1, 2025
Dermatologist reviewed: Natalie Matthews, MD, MPhil, FAAD; Rajiv I. Nijhawan, MD, FACMS, FAAD; and Darrell S. Rigel, MD, FAAD. Reviewer bios.
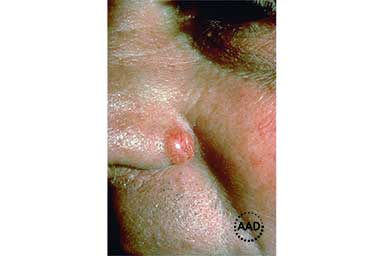
A firm, raised, round growth that’s shiny and pink or red is often a sign of basal cell carcinoma on lighter skin tones.
The firm, raised, round growth on this patient’s skin is basal cell carcinoma.

A firm, raised, round growth that’s brown or black can be a sign of basal cell carcinoma on darker skin tones.

Basal cell carcinoma can look like a firm, round, raised growth that’s the same color as your skin.

This shiny bump is basal cell carcinoma. In darker skin tones, it tends to be black, brown, or blue.

Basal cell carcinoma can have more than one color, as shown here.

Basal cell carcinoma can look like a round area with a dip in the center.

When basal cell carcinoma has a dip in the center, the dip may scab over and bleed.

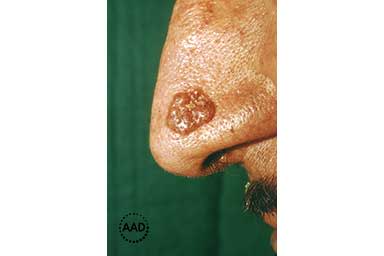
Basal cell carcinoma can look like a rough, scaly patch, and some people develop several patches.

Basal cell carcinoma often appears as a scaly patch on or near an ear.

A spot that looks like a freckle or age spot but feels scaly can be basal cell carcinoma.

A sore that heals and returns or fails to heal can be basal cell carcinoma.
These pictures are meant to give you an idea of what basal cell carcinoma can look like. Keep in mind that you cannot rule out or know whether you have this skin cancer by looking at pictures. If you’re concerned about a spot or growth on your skin, make an appointment to see a board-certified dermatologist. This doctor can examine your skin and tell you the appropriate next step to take.
Related AAD resources
Basal cell carcinoma: From symptoms to treatment: Discover symptoms, how this cancer is diagnosed, and treatment options.
Basal cell carcinoma: Outcome and life after treatment: Find out why most patients have a good outcome and what dermatologists tell their patients after treatment.
Dermatologist reviewer bios
Natalie H. Matthews, MD, MPhil, FAAD
Dr. Matthews is a board-certified dermatologist and Fellow of the American Academy of Dermatology (FAAD). She sees patients at Henry Ford Health in Michigan and is a Clinical Assistant Professor of Dermatology at Michigan State University.
Her areas of expertise include:
Skin cancer
Melanoma
Skin cancer surgery
Moles and other non-cancerous growths
In addition to seeing patients and teaching, Dr. Matthews is Co-director of the Henry Ford Pigmented Lesions Clinic and Co-director of the Henry Ford Cancer Center Melanoma Tumor Board.
Her research interests include:
Melanoma
Skin cancer prevention
Patient education
Rajiv I. Nijhawan, MD, FACMS, FAAD
Dr. Nijhawan is a board-certified dermatologist and board-certified Mohs surgeon. He is a Fellow of the American Academy of Dermatology (FAAD) and the American College of Mohs Surgery (FACMS).
His areas of expertise include:
Mohs surgery
Reconstructive surgery
Surgical treatment for all types of skin cancer
In addition to performing surgery, he is an Associate Professor of Dermatology at the University of Texas Southwestern (UTSW) Medical Center, Director of the Parkland Memorial Hospital Skin Tumor Clinic, and Director (and founder) of the UTSW High Risk Skin Cancer Transplant Clinic. The latter serves people who have received an organ transplant, as anyone living with a transplanted organ has a greatly increased risk of developing skin cancer.
His research interests include:
Skin cancer
Mohs surgery
Patient safety
Darrell S. Rigel, MD, MS, FAAD
Dr. Rigel is a board-certified dermatologist and fellow of the American Academy of Dermatology (FAAD). With over 40 years of experience in the field, Dr. Rigel is well known for his expertise, especially in the areas of:
Melanoma
Early detection of skin cancer
Skin cancer treatment
Passionate about education, Dr. Rigel has trained many dermatologists. He is currently Clinical Professor of Dermatology at the NYU School of Medicine and Adjunct Clinical Professor of Dermatology at UT Southwestern Medical School.
Dr. Rigel is well known for his research and patient care. He co-authored numerous articles that appear in leading medical publications. He co-created the ABCDEs of Melanoma. This easy-to-remember message has helped countless people find this skin cancer early when it’s highly treatable. Today, the ABCDEs of Melanoma are widely used around the world
Written by Paula Ludmann, MS
Paula has more than 20 years of experience writing about skin, hair, and nail conditions for patients and the public.
She enjoys developing easy-to-understand information that people can use to make informed health decisions.
Paula’s passion for creating patient-first information has led to her work being mentioned by Prevention magazine and the Washington Post. She has won numerous awards, including Webbies, Apex Awards, and several awards from professional organizations.
References
Marzuka AG, Book SE. “Basal cell carcinoma: Pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management.” Yale J Biol Med. 2015 Jun 1;88(2):167-79.
McDaniel B, Steele RB. “Basal cell carcinoma.” Updated 2024 Mar 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
National Comprehensive Cancer Network (NCCN). “NCCN guidelines: Basal cell carcinoma.” Version 2.2025, February 7, 2025. Last accessed: July 16, 2025.
Nouri K, Ballard CJ, et al. “Basal cell carcinoma.” In: Nouri K, et al. Skin Cancer. McGraw Hill Medical, China, 2008: 61-81.
Tang JY, Epstein EH, et al. “Basal cell carcinoma and basal cell nevus syndrome.” In: Kang S, Amagai M, et al. Fitzpatrick’s Dermatology (ninth edition). McGraw Hill Education, New York, 2019: 1884-8.
Image credits
Images 1, 2: American Academy of Dermatology, National Library of Dermatologic Teaching Slides 4.0.
Image 3: Used with permission of the American Academy of Dermatology’s Clinical Image Collection.
Images 4, 7, 8, 10, 11, 12: Used with permission of the Journal of the American Academy of Dermatology:
J Am Acad Dermatol. 2019;80:303-17. (4, 7, 8)
JAAD Case Reports 2022;28:11-3. (10)
JAAD Case Reports 2018;4:599-601. (11)
J Am Acad Dermatol. 2014;70(4):748-62. (12)
Images 5, 6, 9: Produced with permission from ©DermNet www.dermnetnz.org 2025.
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?