5 signs your child's mole needs to be checked
Moles on a child’s skin are generally nothing to worry about. New moles appear during childhood and adolescence. As the child grows, the moles will naturally get bigger. It’s also normal for moles on a child’s skin to darken or lighten. Some moles fade away. These changes are common and rarely a sign of melanoma, a type of skin cancer that can begin in a mole.
In fact, melanoma is rare in young children. Even so, there are times when a mole should be checked by a dermatologist just to be sure. Caught early, melanoma is highly treatable.
The following can help you decide when a dermatologist should examine your child.
Changing mole: It's normal for a mole to grow at the same rate as a child. It's also natural for a child's moles to get darker or lighter.
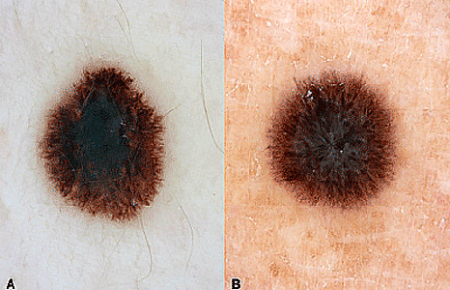
Melanoma on 14-year-old girl's arm
This had been a mole for years, but then it started to change — growing quickly and becoming painful.

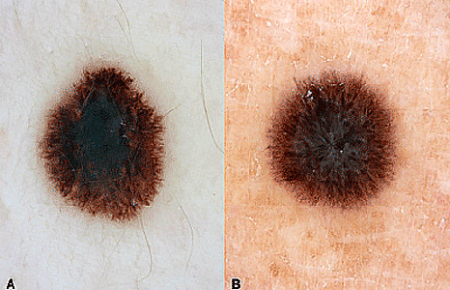
Mole that is dome-shaped, has a jagged border, or contains different colors: If you see a raised, round growth on your child's skin that is pink, red, tan, or brown, it's likely a Spitz nevus. This is a harmless mole that usually appears between 10 and 20 years of age. A child can also be born with this type of mole.
Spitz nevus or melanoma?
This harmless mole is a Spitz nevus (A), which can look at lot like melanoma (B).
Bleeding mole: A raised mole can catch on something and become irritated. If a mole bleeds without reason, however, it should be checked. A mole that looks like an open sore is also worrisome. Bleeding or a break in the skin can be a sign of melanoma.
Many moles: It's normal for a child or teenager to get new moles. By the time a child becomes an adult, it's common to have 12 to 20 moles.
Many moles
Having 50-plus moles increases one’s risk of getting melanoma.

Large mole: Most moles are round (or oval) spots that are smaller than the eraser on a pencil.
Giant mole
The 4-year-old boy has had this giant mole since birth.

Checking moles in childhood can create a healthy, lifelong habit
Looking at moles and getting a worrisome one checked can teach your child how important it is to know your moles. If your child starts do this at an early age, it’s likely to become a lifelong habit.

Protecting your child’s skin from the sun now can reduce her risk of getting melanoma and other skin cancers. Learn simple, effective ways to protect your child’s skin.
Related AAD resources
Images
Spitz nevus: Image used with permission of Journal of the American Academy of Dermatology: J Am Acad Dermatol 2015;72:47-53.
Many moles: Image used with permission of Journal of the American Academy of Dermatology: J Am Acad Dermatol 2015;73:491-9.
Giant mole: Image used with permission of Journal of the American Academy of Dermatology: J Am Acad Dermatol 2009;61:766-74.
Other images: Getty Images
References
Cordoro KM, Gupta D, et al. “Pediatric melanoma: Results of a large cohort study and proposal for modified ABCD detection criteria for children.” J Am Acad Dermatol 2013;68:913-25.
Lovett, A, Maari C, et al. “Large congenital melanocytic nevi and neurocutaneous melanocytosis: One pediatric center’s experience.” J Am Acad Dermatol 2009;61:766-74.
Mitkov M, Chrest M, et al. “Pediatric melanomas often mimic benign skin lesions: A retrospective study.” J Am Acad Dermatol 2016;75:706-11.
Scope A, Marchetti M, et al. “The study of nevi in children: Principles learned and implications for melanoma diagnosis.” J Am Acad Dermatol 2016;75:813-23.
Wynnis LT, Hsu JW, et al. “Pediatric ‘‘STUMP’’ lesions: Evaluation and management of difficult atypical Spitzoid lesions in children.” J Am Acad Dermatol 2011;64:559-72.
 Atopic dermatitis: More FDA-approved treatments
Atopic dermatitis: More FDA-approved treatments
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 How to trim your nails
How to trim your nails
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Tattoo removal
Tattoo removal
 Scar treatment
Scar treatment
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?