Melanoma treatment
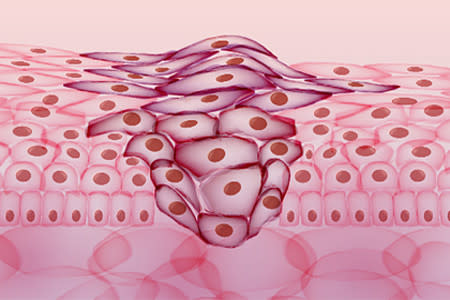
When treating melanoma, doctors strive to remove all the cancer. Because surgery (aka surgical removal) tends to be the most effective way to do this, a patient who has melanoma will often have surgery. If you have an early melanoma, your dermatologist can often perform this surgery during an office visit. This may be the only treatment you need.

Melanoma: Diagnosis and treatment
Find information about the different treatments and life expectancy.

Treatment: Head and neck
Melanoma can behave differently on the head and neck. Here’s what a treatment plan may look like.
When melanoma spreads to the brain
Attacking the cancer with different types of treatment can improve how well each works.
 Molluscum contagiosum: How to safely treat it
Molluscum contagiosum: How to safely treat it
 Biosimilars: 14 FAQs
Biosimilars: 14 FAQs
 Practice Safe Sun
Practice Safe Sun
 Relieve uncontrollably itchy skin
Relieve uncontrollably itchy skin
 Fade dark spots
Fade dark spots
 Untreatable razor bumps or acne?
Untreatable razor bumps or acne?
 Laser hair removal
Laser hair removal
 Scar treatment
Scar treatment
 Botox
Botox
 Free materials to help raise skin cancer awareness
Free materials to help raise skin cancer awareness
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 What is a dermatologist?
What is a dermatologist?